Image credit: Proxima Studio | Stock.Adobe.com
Continuous glucose monitoring (CGM) has emerged as an innovative tool in diabetes management and is particularly beneficial for pregnant women. CGM systems utilize wearable sensors that continuously track glucose levels in interstitial fluid, providing real-time data and trends about a patient’s glucose levels throughout the day. This continuous flow of information allows for more nuanced adjustments to insulin therapy and dietary management compared to traditional blood glucose monitoring methods that only provide snapshot measurements.
The importance of maintaining tight blood sugar control during pregnancy cannot be overstated. Proper blood sugar control is important to minimize the risk of pregnancy complications such as pre-eclampsia, caesarean section, macrosomia (a baby with a high birth weight), and to reduce the risk of long-term complications in the child, such as increased risk of obesity and diabetes. It is very important to minimize health problems.Indicators such as hemoglobin A1c (HbA1c) and blood sugar levels are the cornerstone of diabetes management. However, achieving and maintaining target glycemic control is especially important during pregnancy. Hyperglycemia, or high blood sugar levels, can have negative effects on mother and baby, making reliable and effective blood glucose monitoring systems an essential part of diabetes care during pregnancy.1
Despite the clear advantage of CGM in providing comprehensive glucose data, there have been concerns about its accuracy and usefulness, particularly in the pregnant population. This concern stems from the need for more definitive data regarding her CGM use during pregnancy and the potential for variability in sensor accuracy. Nevertheless, the rationale behind the use of CGM, namely that it provides a more detailed picture of blood glucose levels throughout the day, makes a compelling case for incorporating CGM into the management plan of a pregnant woman with diabetes. An example is shown. As CGM technology continues to advance and more research becomes available, the role of CGM in optimizing blood sugar control during pregnancy and ensuring healthier outcomes for mother and baby will become increasingly essential. It may become.
CGM during pregnancy: benefits and considerations
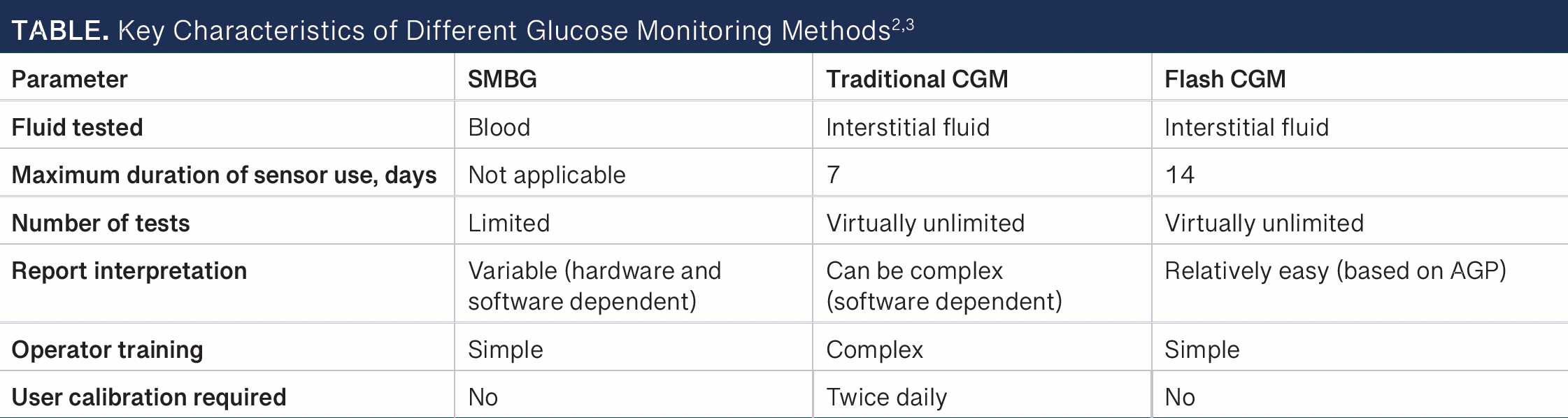
The advent of CGM systems has led to major advances in diabetes management, especially in pregnant women. Unlike traditional self-monitoring of blood glucose (SMBG), which relies on intermittent finger prick tests, CGM provides a more comprehensive picture of blood glucose levels throughout the day by measuring interstitial blood glucose levels.of table It highlights important features of different blood glucose monitoring methods.2, 3 Although this measurement is slightly delayed (5 to 15 minutes behind blood glucose), it provides up to 288 readings per day and allows detailed monitoring of blood sugar fluctuations that SMBG cannot provide.
AGP, ambulatory blood glucose profile; CGM, continuous glucose monitoring; SMBG, self-monitoring of blood sugar.
The 2017 CONCEPTT trial (NCT01788527) was a pivotal moment in research on CGM use during pregnancy. Pregnant women with type 1 diabetes using CGM demonstrated mild improvement in HbA1c They spent more time within their target blood glucose range and had fewer hypoglycemic events compared to using SMBG.Four Of note, this trial demonstrated significant benefits for neonatal health outcomes, including longer gestational age deliveries, reduced neonatal intensive care unit (NICU) admission, reduced incidence of neonatal hypoglycemia, and shorter length of hospital stay. has also become clear. These findings highlight that CGM not only optimizes maternal glycemic control but also has the potential to improve neonatal health.Four
Recent studies have highlighted the importance of the time-in-range (TIR) metric, which measures the period during which a patient’s blood glucose level is within the target range (63 to 140 mg/dL).Five Studies have consistently shown a strong correlation between increased TIR and improved pregnancy-related health outcomes, including lower risks of older births, gestational hypertension, and NICU admissions.6-8
The American Diabetes Association has updated its standards of care to recommend the use of CGM in pregnancies complicated by type 1 diabetes, citing limited but promising data for patients with type 2 diabetes or gestational diabetes. Recommendations for the use of her CGM for type 2 diabetes and gestational diabetes during pregnancy are still evolving, but new research suggests similar benefits across these groups.Five
Introducing CGM in diabetes management plans
Incorporating CGM into a diabetes management plan during pregnancy requires careful consideration of its benefits and limitations. CGM reduces the need for frequent finger-prick blood sugar tests, but requires calibration with SMBG to ensure accuracy. Nevertheless, the comprehensive data provided by CGM can significantly enhance glycemic control strategies. It enables real-time monitoring of blood sugar levels, facilitating immediate adjustments to insulin dosage and dietary management. CGM enables a more tailored approach to diabetes management, aiming to minimize hyperglycemia and prevent hypoglycemia by tracking overnight and postprandial blood sugar levels.
Pharmacists play an important role in incorporating CGMs into diabetes treatment plans for pregnant patients. Pharmacists must assess each patient’s specific needs, preferences, and risk factors to determine the most appropriate method for using CGMs. Education about the use, interpretation, and limitations of CGM data is essential to enable patients to become active participants in their treatment.
About the author
Bader Alghamdi, PharmD, BCPS; is a PGY2 outpatient pharmacy located in the Department of Pharmacy Practice at the Texas A&M Irma Lerma Rangel School of Pharmacy in Kingsville.
Samantha Owendalski I am a PharmD candidate in the Department of Pharmacy Practice at the Texas A&M Irma Lerma Rangel School of Pharmacy in Kingsville.
Sinonso Paul She is a PharmD candidate in the Department of Pharmacy Practice at the Texas A&M Irma Lerma Rangel School of Pharmacy and an MBA candidate at Texas A&M University in Kingsville.
Omolala Farade She is a PharmD candidate in the Department of Pharmacy Practice at the Texas A&M Irma Lerma Rangel School of Pharmacy and an MBA candidate at Texas A&M University in Kingsville.
Sarah Rogers, Pharm.D., BCPS; He is a clinical assistant professor of precision medicine and ambulatory care at the Texas A&M Irma Lerma Rangel College of Pharmacy in Kingsville, a clinical specialist at Texas A&M Health Family Care, and a co-founder of the American Pharmacovigilance Association.
As research continues to evolve, the evidence supporting the use of CGM in pregnancy becomes increasingly convincing. This offers a promising avenue to improve maternal and neonatal outcomes by enabling more precise and individualized management of diabetes. With further research and technological advancements, CGM has the potential to become a standard component of care for all pregnant women with diabetes, ensuring healthier pregnancies and improved outcomes for both mother and baby.
References


