Wireless and soft smart contact lens system for tear glucose monitoring
Our SCL is designed to provide the ability to monitor the glucose level in tears and to transmit this information wirelessly to the user’s smartphone. Figure 1b shows the overall schematic illustration of this real-time glucose monitoring SCL system, composed of a glucose sensor and wireless communication components, in the form of a soft contact lens. Among the standard wireless communication technologies, near-field communication (NFC) can be suitable for the smart contact lens because it allows a wireless supply of power to a sensor for its battery-free operation, and it allows the wireless transmission of data with sufficient bandwidth. The detailed fabrication procedure is described in Supplementary Fig. 1 and the Methods section. After locating the stretchable integration of all of the components of the device on a flat elastic film, the molding of the resulting flat sample (with devices) into the curved lens shape by injecting a precursor of silicone elastomer (Interojo®), which is a commercially available material for a soft contact lens, completed the fabrication of our SCL. During this molding step, the selective area of the glucose sensor was open and locally uncovered by the lens material to allow its physical contact with tears. In this way, all of the electronic devices could be embedded inside the soft contact lens with this opening remaining for the sensor (Supplementary Fig. 2). The NFC system of our SCL was able to wirelessly transmit the measured glucose data to a smartphone. The smartphone could display the measured TG concentration in real-time through the smartphone application, and the data were stored in a database.
The SCL was designed for the continuous measurement of the TG concentration using the electrochemical system of the glucose sensor. Glucose oxidase (GOx) was immobilized along with chitosan on the working electrode (WE), and it reacted with glucose to generate gluconolactone and H2O2 as products (Fig. 1c). Prussian blue (PB) on WE acted as an artificial peroxidase that facilitates the reduction of H2O2 that resulted from the reaction between glucose and GOx48. For the amperometric detection of glucose, a potential of −0.1 V (vs Ag/AgCl) was chosen based on the cyclic voltammetry (CV) results in Supplementary Fig. 3. As shown in Fig. 1d, e, the relative change in the current response was measured at various glucose concentrations. The concentration of glucose increased linearly with a sensitivity of 1% change in reduction current per 0.047 mM and a detection limit of 0.02 mM, demonstrating that this developed glucose biosensor could detect glucose variations in human tears (0.18–0.7 mM)34. This device exhibited good selectivity in the presence of physiologically relevant interferences (Supplementary Fig. 4a), and it showed negligible differences in various physiological tear pH values49, from 6.4 to 7.6 (Supplementary Fig. 4b). Also, it provided 21 days of long-term stability at room temperature (22 °C) (Supplementary Fig. 4c).
Remote monitoring of the real-time glucose concentration was performed through the NFC function between SCL and a smartphone, with the stretchable integration of a commercial NFC chip (NHS 3152, NXP Semiconductors, thickness: 200 µm after polishing), the serpentine antenna, capacitor, and the glucose sensor. To match the standardized resonance frequency of NFC (13.56 MHz), as illustrated in Fig. 1f, an 81 pF capacitor was integrated into the stretchable serpentine antenna that was designed for this resonance frequency based on calculations using the High-Frequency Structure Simulator (HFSS) program. The resulting SCL exhibited a resonance frequency centered at 13.56 MHz (Fig. 1g). When the antenna supplies power to the wireless circuit through inductive coupling with a smartphone, a Digital-to-Analog Converter (DAC) in the NFC chip applied a constant voltage (−0.1 V) to the glucose sensor for the electrochemical sensing (Fig. 1h). The resulting current response was read by the Current-to-Digital converter (I2D) with 100 ms integration time, which was sufficient to monitor the changing TG, and the current data were transmitted wirelessly to the smartphone. In a smartphone application, the concentration of glucose calculated from the current value that is detected could be updated every second.
Successful demonstration of the integrated SCL biosensor on the eye of a mannequin was performed for wireless glucose sensing with a smartphone, and it showed only 3% error or less with the reference concentration of glucose (Supplementary Fig. 5 and 6). The biocompatibility of SCL was evaluated in human corneal cells (HCE-2) and human conjunctival cells (HCECs) using a LIVE/DEAD assay kit and Cell Counting Kit-8 (CCK-8). Supplementary Fig. 7 shows that 97.88 ± 1.82% of HCE-2 and 95.28 ± 1.67% of HCECs did not exhibit significant cytotoxicity compared to controls. Calcein-AM/ethidium homodimer-1 double staining also revealed no significant dead cells, confirming negligible cytotoxicity (Supplementary Fig. 8). These results indicate that our SCL satisfied the cytotoxicity standard of over 80% for medical devices (ISO 10993-5).
Effects of reflex tears on the correlation between TG and BG
There has been a continuing controversy about the clinical significance of TG as a biomarker for diabetic mellitus, especially, due to variations in tear composition caused by physical stimulation of the eye, which can induce reflex tears and cause fluctuations in TG. For example, conventional methods of collecting tears (e.g., filter paper and Schirmer strip) elicit reflex tears because these sharp tips come into direct contact with the ocular surface. However, the SCL is a relatively soft, stretchable, and biocompatible device that can continuously and comfortably contact tear fluid, and it is expected to minimize tear stimulation when worn. As shown in Fig. 2a, the changes in tear volume (TV) and TG were monitored continuously after our SCLs were worn on the eyes of four normal rabbits. Here, TG was measured through the SCL every 20 s from the time of wearing the SCL, and TV was measured every minute through a strip meniscometry tube (SMTube) by absorbing tear film meniscus (Supplementary Fig. 9a). As plotted in Fig. 2b, c, when the SCL was worn, both TV and TG levels immediately increased (due to reflex tearing) and then reduced rapidly again close to their initial states. These rapid recoveries of both TG and TV appeared about 160 and 135 s, respectively, after wearing the SCL (Fig. 2d). Then, TG and TV became stabilized without significant fluctuations, indicating negligible additional eye irritation from wearing the SCL. The disturbances of the TG and TV levels only occurred for a short time when the SCL was being worn. Therefore, in all of the following in vivo experiments, TG was measured by giving sufficient stabilization time of 10 min after wearing the SCL.
a Photograph showing the sequence for TG and TV monitoring after wearing smart contact lens (SCL). Scale bars, 1 cm. b Real-time measurement of TV when wearing SCL in normal rabbits (n = 4). c Real-time measurement of TG when wearing SCL in normal rabbits (n = 4). d, Comparison of TG level recovery time and TV recovery time after SCL wearing (n = 4). For (b–d) each data point represents the average of four normal rabbits, and the error bars indicate mean ± standard error of the mean. e Timeline of continuous measurement of blood glucose (BG), TG and TV along with conjunctival stimulation. f Photograph of external stimulation to the conjunctiva of rabbit using a von Frey filament. Scale bars, 1 cm. g Average of SMTube scores of four rabbits as a function of stimulating force (n = 4). Each data point represents the average of four normal rabbits, and the error bars indicate mean ± standard error of the mean. h Representative data of monitoring TG and BG levels (top) and relative changes in TV along with mechanical stimulation (bottom).
Further, we investigated the effect of physical stimulation-induced reflex tears on the correlation between TG and BG in rabbit models while wearing the SCL. As shown in Fig. 2e, continuous measurements of the levels of BG, TG, and TV were performed in four normal rabbits with mechanical eye stimulation. For the external stimulation to the conjunctiva, the von Frey filament, which can provide constant calibrated force, was used to induce the additional reflex tear fluid (Fig. 2f and Supplementary Fig. 9b). The strength of the stimulation force that can induce sufficient reflex tearing while minimizing conjunctival damage was determined to be 1.4 gf, and no significant increase in TV occurred with stronger forces (Fig. 2g and Supplementary Fig. 10). Figure 2h is the resulting representative plot among four normal rabbits. After stimulation on the SCL-worn conjunctiva, TV increased rapidly, along with a TG spike. It is consistent with the findings from previous studies that mechanical stimulation can cause glucose to leak directly from the interstitial space or epithelial cells into the tear fluid20,41. After the spike, both TG and TV soon recovered. The same trend of variations was observed in the other three rabbits (Supplementary Fig. 11). As shown in Supplementary Fig. 12, the average recovery times for TG and TV in the four rabbits were ~300 s and 260 s, respectively. The recovery time refers to the time taken from the secretion of reflex tears to the complete clearance of the effects of the reflex tears due to the repeated secretion and drainage processes of the tears (i.e., tear circulation)50. It implies that, although TG measurement after this stimulation can compromise its correlation with BG, it can be recovered soon. Note that SCL allows us to obtain stable TG values in a continuous way while wearing and when external stimulation is not present, and even when it occurs unexpectedly, TG can recover soon and allows us to obtain reliable TG values. Such a feature enables the in-depth investigation of the correlation between TG and BG in a continuous manner with in vivo models.
In vivo correlation analysis between BG and TG with normal and diabetic rabbit models
In this section, we present the availability of SCL for TG monitoring and the establishment of a correlation analysis method between BG and TG by measuring both in a real-time and continuous way via the oral glucose tolerance test (OGTT) in normal rabbits, as well as via the intravenous glucose tolerance test (IVGTT) in normal and diabetic rabbits (Fig. 3a and Supplementary Movie 1). Initially, we conducted studies to validate the reliability of SCL and to establish a correlation analysis method using a normal rabbit model. In these studies, rabbits with fasting were anesthetized to minimize the changes in TG through additional movement or stimulation. When the BG level was stable, the TG level of both eyes showed a normal range of 0.45–0.48 mM without any significant variations, indicating that the TG level of one of both eyes can represent the actual TG level of the rabbit if there is no additional stimulation of the eyes (Supplementary Fig. 13). Next, an OGTT was conducted on normal, fasting rabbits to evaluate the relationship between TG and BG by observing variations in glucose levels. A 50% (w/w) glucose-concentrated solution at 3.0 g kg−1 of body weight was orally administered to four normal rabbits. The BG level was measured at 10-min intervals using a glucometer concurrently with continuously measuring TG using the SCL (Fig. 3b). In the fasting state, rabbit subject 1 showed 0.423 mM of TG and 6.21 mM of BG, which were within the normal range of TG36 and BG51 for rabbits. After oral administration of the glucose solution, the TG and BG levels increased gradually and showed the highest levels of 1.059 mM and 11.04 mM respectively, and then the levels decreased gradually to 0.614 mM and 6.58 mM, respectively, under the influence of insulin via glucose homeostasis52 (Fig. 3c). All four rabbits showed similar trends of up-and-down in both TG and BG levels, but each rabbit had different values of TG and BG. These different values were due to the variations in the glucose metabolism and metabolic actions of insulin among individual rabbits even though they had consumed the same amount of glucose per weight (Supplementary Fig. 14). Also, TG values reflected the trend of BG with certain delayed time in all four rabbits. Such phenomena often occur in non-invasive biofluids, such as sweat, and saliva and the delayed time corresponds to the time for the biomarkers to diffuse from the blood vessels to the biofluids53,54,55. We called it “lag time” and calculated it for each rabbit to identify how it can impact Pearson’s correlation coefficient between BG and TG. The correlation coefficient and regression line between TG and BG levels varied depending on the value of the applied lag time (Supplementary Fig. 15). As shown in Fig. 3d, the correlation coefficient was plotted further with the lag time ranges from 0 to 25 min in increments of 1 min, demonstrating that accurate estimation of lag time is crucial for the higher degree of correlation between TG and BG. The coefficient at 14 min showed the highest value of 0.987, indicating that 14 min was the most precise lag time for the tested rabbit. In this way, the determination of personalized lag times for the other three rabbits was performed, showing 14, 13, and 13 min, respectively (Supplementary Fig. 16). All measured OGTT data were plotted together for four rabbits by applying the personalized lag time for each rabbit. This resulted in 0.944 of Pearson’s correlation coefficient, indicating a strong linear relationship between TG and BG (Supplementary Fig. 17).
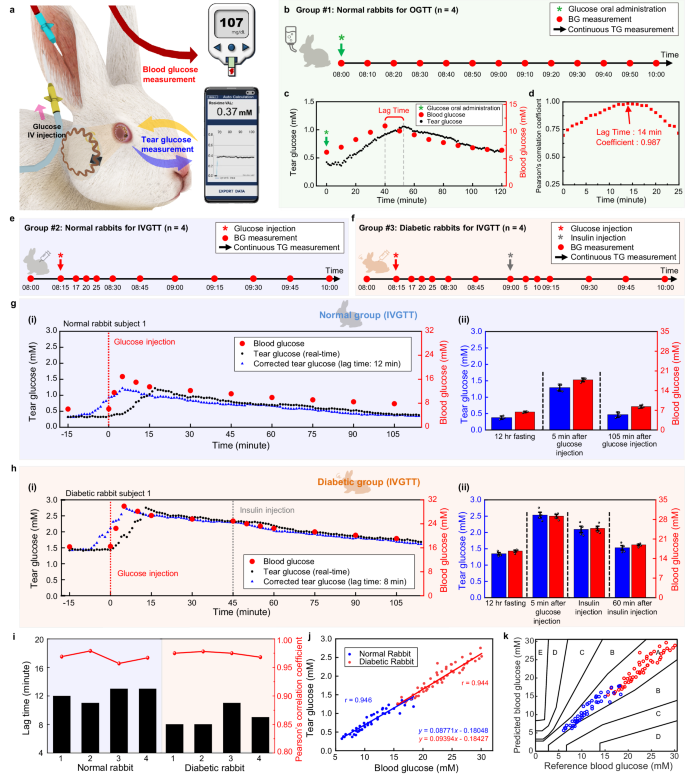
a Schematic illustration of the simultaneous measurement of TG and BG during IVGTT in a rabbit model. b Timeline of BG, and TG measurement after oral administration of glucose in normal rabbits. c, Representative data of monitoring TG and BG in normal rabbits after oral administration of glucose. d Pearson’s correlation coefficient between TG and BG as a function of lag time. e Timeline of continuous measurement of TG and BG after glucose intravenous (IV) injection for normal rabbits. f Timeline of continuous measurement of TG and BG after IV injection of glucose and insulin for diabetic rabbits. g Representative real-time data of TG and BG in a normal rabbit after IV injection of glucose. (i), Real-time monitoring of TG (black dots), BG (red dots), and corrected TG data (blue dots) of a normal rabbit. (ii), Comparison between the average of TG and BG in four normal rabbits before and after the injection of glucose, and the error bars indicate mean ± standard error of the mean. h Representative real-time data of TG and BG in a diabetic rabbit after IV injection of glucose and insulin. i Real-time monitoring of TG (black dots), BG (red dots), and corrected TG data (blue dots) of a diabetic rabbit. (ii), Comparison between the average of TG and BG in four diabetic rabbits before and after injection of glucose and insulin, and the error bars indicate mean ± standard error of the mean. i Lag time identification through the Pearson’s correlation coefficient in rabbit models. j Comprehensive Pearson’s correlation analysis of 4 normal rabbits and FOUR diabetic rabbits. k Comprehensive Parkes error grid analysis of four normal rabbits and FOUR diabetic rabbits.
We further investigated the correlation between TG and BG via IVGTT in normal and diabetic rabbits. The diabetic rabbits were prepared by streptozotocin (STZ) treatment, which is fatal to the insulin-producing beta cells of the pancreas. Over the course of inducing diabetes, the rabbits lost weight and had increases in their fasting BG values (Supplementary Fig. 18). To confirm the induction of diabetes in the rabbit models, we performed histological analysis of the pancreatic islets after completing the in vivo experiments. Supplementary Fig. 19 displays immunostaining images for glucagon and insulin in the pancreatic islet. The pancreatic islet area of diabetic rabbits was reduced by ~97.70% compared to normal rabbits, indicating successful induction of diabetes in rabbit models. In detail, the normal rabbits had an area of 766.41 ± 150.55 µm2, whereas the diabetic rabbits had an area of 17.63 ± 8.70 µm2.
After anesthetizing the 12-h-fasted rabbits, a 50% concentrated glucose solution, at a dosage of 1.0 g kg−1 of body weight, was injected intravenously through the marginal ear vein. The IV injection of glucose can minimize the variables of glucose absorption rate that may occur in oral administration and can reduce urinary loss of glucose and maximize insulin response56. Therefore, the IV injection method enables the clear and effective spike of the glucose in the animal models and offer the advantage of systematic analysis of correlation in TG and BG. After wearing the SCL, TG was monitored continuously, and BG was measured through the auricular artery at the designated time (Fig. 3e). An IV injection of glucose was performed via the marginal ear vein. In diabetic rabbits only, 0.5 U kg−1 of insulin was injected 45 min after glucose injection to lower their glucose levels (Fig. 3f). In the case of the normal rabbit model, a representative result among four normal rabbits is shown in Fig. 3g-(i). Normal rabbit subject 1 showed a BG level of 6.06 mM in its fasting state, which was within the BG range of normal rabbits, and it increased to 16.89 mM within 5 min after the glucose IV injection. Subsequently, it decreased gradually to 7.84 mM at 105 min after glucose injection due to glucose homeostasis. Simultaneously, TG also showed a normal fasting level at 0.321 mM and increased to 1.22 mM with glucose injection. Further, it also decreased to 0.369 mM at the end of the experiment, following the dynamic behavior of BG with a certain lag time. Similar trend also was observed in the other three normal rabbits (Supplementary Fig. 20). The lag time of each rabbit between TG and BG was determined as 12, 11, 13, and 13 min, respectively. After the correction of TG data with the lag time value (blue dot), the tendency of TG appeared very similar to the change in the BG level. Figure 3g-(ii) shows the summarized average values for BG and corrected TG from all four rabbits through the course of IGVTT for normal rabbits. For the diabetic rabbit model, a representative result among four diabetic rabbits is shown in Fig. 3h-(i). Despite being in a fasting state, it showed an abnormally high BG level of 16.32 mM, confirming the difficulty in maintaining glucose homeostasis due to damage in beta cells, and further increased to 29.89 mM after 5 min of glucose IV injection. The BG level was then progressively reduced by secreted insulin, which was not as effective as in normal rabbits, but remained much higher than the normal range. Insulin was injected 45 min after the glucose injection to further lower the glucose level in the blood. The BG level started to decrease at a faster rate to 19.09 mM after 60 min of insulin injection, but still out of the normal BG range. The TG level started at 1.434 mM in the fasting state, spiked up to 2.755 mM, and then recovered to 1.687 mM at the end. TG also showed a similar trend to BG with a certain lag time, and the other three diabetic rabbits also exhibited the same trend (Supplementary Fig. 21). The corrected TG data (blue dot) by applying 8, 8, 11, and 9 min of personalized lag time to each diabetic rabbit showed high correspondence with BG. Figure 3h-(ii) presents the average values of corrected TG and BG in these four diabetic rabbits. Figure 3i displays the difference in the lag time among all of the rabbit models. From these results, we concluded that personalizing the lag time is crucial and plays an essential role in accurate identification of the correlation between TG and BG. Pearson’s correlation coefficient, calculated by plotting all measured values from 8 rabbits, was high enough with the values of 0.946 in the normal group and 0.944 in the diabetic group (Fig. 3j). We introduced Parkes Error Grid Analysis to evaluate the accuracy of the predicted BG based on TG. The Parkes Error Grid is a commonly used method to assess the clinical accuracy of predicted BG, and reasonable predictions can be made when the predicted BG belongs to Zones A and B57. As presented in Fig. 3k, all plotted data points from normal (blue dots) and diabetic (red dots) rabbits were located in the A and B regions, which represent that the prediction of BG level with measured TG data can be clinically accurate.
In vivo correlation analysis between BG and TG with normal and diabetic beagle models
To further analyze the correlation between the TG and BG levels across different species, an IVGTT with SCL was conducted on the beagle model (Fig. 4a, b, and Supplementary Movie 2). The beagle is an omnivorous animal that has a diet pattern that is more similar to humans than rabbits. Therefore, conducting correlation analysis using the beagle model may provide more precise predictions for the human model. Beagles were injected with STZ to induce diabetes. Induction was confirmed by changes in body weights (Supplementary Fig. 22) and histological analysis after all experiments. Supplementary Fig. 23 shows a reduction in pancreatic islet area of 86.51% in diabetic beagles compared to normal beagles (normal beagles: 1506.51 ± 271.80 µm2, diabetic beagles: 203.17 ± 70.11 µm2), indicating successful induction of diabetes.
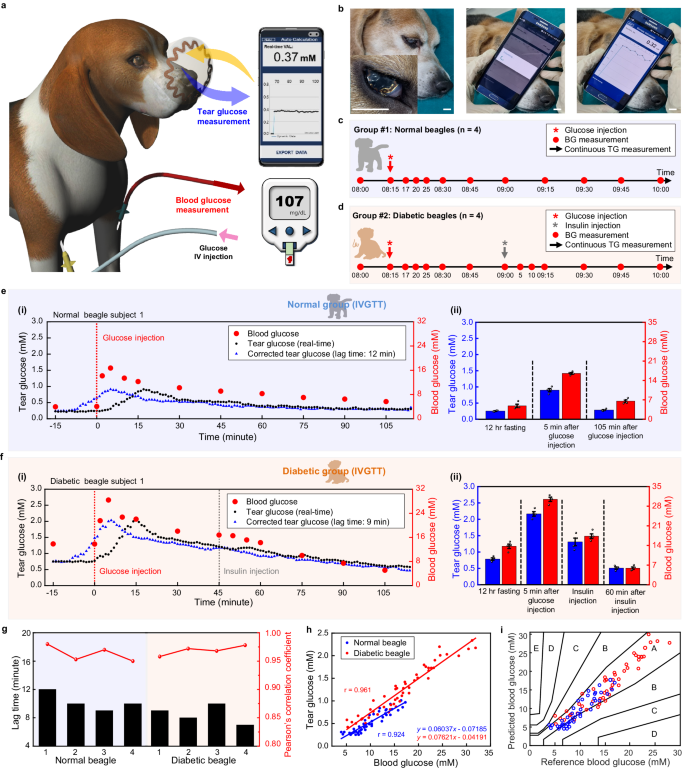
a Schematic illustration of simultaneous measurement of TG and BG during intravenous glucose tolerance test (IVGTT) in a beagle model. b Photographs of simultaneous measurement of TG measurement via SCL. Scale bars, 1 cm. c Timeline of continuous measurement of TG and BG at designated time after glucose intravenous (IV) injection in normal beagles. d Timeline of continuous measurement of TG and BG at designated time after IV injection of glucose and insulin in diabetic beagles. e Representative real-time data of TG and BG in a normal beagle after IV injection of glucose. (i), Real-time monitoring of TG (black dots), BG (red dots), and corrected TG data (blue dots) of a normal beagle. (ii), Comparison between the average of TG and BG in four normal beagles before and after injection of glucose, and the error bars indicate mean ± standard error of the mean. f Representative real-time data of TG and BG in a diabetic beagle after IV injection of glucose and insulin. (i), Real-time monitoring of TG (black dots), BG (red dots), and corrected TG data (blue dots) of a diabetic beagle. (ii), Comparison between the average of TG and BG in four diabetic beagles before and after injection of glucose and insulin, and the error bars indicate mean ± standard error of the mean. g Lag time identification through the Pearson’s correlation coefficient of every beagle models. h Comprehensive Pearson’s correlation analysis of four normal beagles and four diabetic beagles. i Comprehensive Parkes error grid analysis of four normal beagles and four diabetic beagles.
After wearing SCL, TG was monitored continuously, and BG was measured via the cephalic vein at the designated time points (Fig. 4c). The IV injection of glucose was conducted via the foreleg vein after anesthetizing. For diabetic beagles only, 0.5 U kg−1 of insulin was injected 45 min after glucose injection (Fig. 4d). As a result of IVGTT, Fig. 4e-(i) shows the representative TG and BG data for a normal beagle subject 1. The BG levels increased rapidly from a baseline of 3.94 mM, which was within the reported normal range for beagles32, then reached a maximum value of 16.72 mM at 5 min after the glucose injection. Subsequently, it gradually decreased to 5.67 mM approaching the normal range. In the case of TG, it was at a fasting level of 0.24 mM showing a similar value with the reported normal beagle’s TG range32. TG further increased to 0.91 mM after the IV glucose injection and then decreased to 0.279 mM after 105 min due to the action of insulin. Similar results were observed in the other three normal beagles (Supplementary Fig. 24). The lag time derived from the measured data of each normal beagle was 12, 10, 9, and 10 min, respectively. The corrected TG data (blue dot) appeared very similar to the BG data. Figure 4e-(ii) presents the summary of IVGTT by showing the average values of the corrected TG and BG from four normal beagles. A representative result among four diabetic beagles is shown in Fig. 4f-(i). An abnormally high value of fasting BG level was shown as 13.83 mM, proving successful induction of diabetes. The maximum level of 28.39 mM was observed 5 min after glucose IV injection. Then, the BG level started to decrease continuously due to glucose homeostasis, but it was not effective enough to bring the BG level to the normal range. Therefore, additional insulin was administered 45 min after the glucose injection to lower the BG level. Subsequently, the glucose continued to decrease and reached the normal range of 5.11 mM after approximately 105 min33. In the case of TG, the fasting value was 0.75 mM, which then increased to maximum level of 2.03 mM, and further decreased to 0.58 mM, following the trend of BG with a certain lag time. And this tendency also was observed in each of the other three diabetic beagles (Supplementary Fig. 25). The corrected TG data (blue dot) applied 9, 8, 10, and 7 min of lag time to each diabetic beagle also appeared very similar to the BG data. As shown in Fig. 4f-(ii), the average values of the corrected TG and BG in four diabetic beagles were summarized. Figure 4g shows that lag time differences also appeared between individual beagles. The resulting Pearson’s correlation coefficients are 0.924 and 0.961 in the normal and diabetic groups, respectively (Fig. 4h). In the Parkes Error Grid, all data points for normal (blue dots) and diabetic (red dots) beagles are located in the A and B regions, indicating that the prediction of BG level with measured TG data is clinically correct and shows high predictive accuracy (Fig. 4i).
Animal species are classified into carnivores, herbivores, and omnivores based on their diet, and it is known that glucose metabolism differs depending on the species58,59. To investigate the correlation between TG and BG among animal species, we conducted a comparative analysis with the experimental results of rabbits and beagles. There were differences in the lag time among individuals in all models, highlighting the importance of identifying the personalized lag time of each animal for proper correlation analysis. In addition, the lag time values in the diabetic model for both rabbits and beagles were relatively shorter than those in the normal model, regardless of individual differences or species. Diabetes can increase tear osmolarity, alter ion transport, and affect blood flow rate around the eyes, thereby promoting glucose diffusion across the blood-tear barrier20,60,61.
We compared the ratio between TG and BG (TG/BG) obtained from Pearson’s correlation analysis, resulting in values of 0.08771, 0.09394, 0.06037, and 0.07621 for normal rabbit, diabetic rabbit, normal beagle, and diabetic beagle, respectively. Rabbits exhibited slightly higher TG/BG ratios for both normal and diabetic groups compared to beagles, indicating differences in the partitioning ratio of glucose between tears and blood among species. The diabetic groups for both species also showed higher TG/BG ratios than the normal group, supporting the notion that diabetes can induce variations in the blood-tear barrier, affecting the transport of glucose across it20,60,61.
Human pilot study for correlation analysis between TG and BG
To investigate the correlation analysis using SCL in humans, we conducted a human pilot study involving both ten healthy human participants and ten diabetic human participants (Supplementary Figs. 26 and 27). Figure 5a and Supplementary Movie 3 present a healthy 26-year-old male participant wearing our SCL and then measuring the TG level using a smartphone wirelessly. We have obtained consent for the individual to appear in the images. After wearing the SCL, under fasting conditions, healthy human participants were asked to drink a soft drink containing 54 g of sugar for OGTT. In the case of participants with diabetes, soft drinks were replaced with nutritional beverages, considering the potential adverse effects of soft drinks on diabetic patients during the experimental period based on physician’s recommendation. After drinking, TG was measured continuously for 120 min, and the BG level also was measured using a glucometer with 5-min intervals. This testing procedure was conducted for 5 days on every other day, day 1, 3, and 5 (Fig. 5b). As shown in Fig. 5c, the representative result among the ten healthy participants, the fasting BG levels of a healthy participant were 5.05, 5.83, and 5.16 mM on day 1, 3, and 5, respectively, which are within the normal BG range. After drinking the soft drink, the BG levels increased up to 9.16, 9.44, and 8.99 mM on day 1, 3, and 5, respectively. And then gradually decreased, returning to baseline under the influence of general glucose homeostasis after 120 min. The fasting state TG levels of a normal participant were 0.329 mM, 0.376 mM, and 0.379 mM on day 1, 3, and 5, respectively, showing values similar to the reported TG range of human34. After consuming sugary drink, the TG levels increased to 0.616 mM, 0.621 mM, and 0.573 mM, and then decreased to 0.379 mM, 0.41 mM, and 0.405 mM. Although there were some individual differences, TG levels showed similar trends to BG levels in all participants (Supplementary Fig. 28). The fasting BG levels in a diabetic participant were slightly higher than those of normal participant, measuring 6.01, 6.63, and 6.18 mM on day 1, 3, and 5, respectively (Fig. 5d). After drinking the nutritional beverage, the BG levels increased up to 9.21, 9.55, and 9.29 mM on day 1, 3, and 5, respectively. The BG level did not return to the baseline within 120 min. This reflects a deficiency in the metabolic actions of insulin in diabetic patients62. Fasting TG levels in the diabetic participants were slightly higher than those of normal participants, showing 0.432, 0.474, and 0.423 mM on day 1, 3, and 5, respectively. The values increased to 0.57, 0.576, and 0.564 mM and then decreased to 0.499, 0.525, and 0.48 mM on day 1, 3, and 5, respectively. The TG levels followed the trend of BG levels with certain lag time, and the other nine diabetic participants exhibited similar results (Supplementary Fig. 29). Although the lag time varied randomly among individuals, the lag time, determined for one individual, was nearly remained constant on day 1, 3, and 5, regardless of whether the participants were healthy or diabetic (Fig. 5e and Supplementary Fig. 30), suggesting the personalized lag time may not be an instantly changing feature, rather be a maintaining feature over a certain period of time.
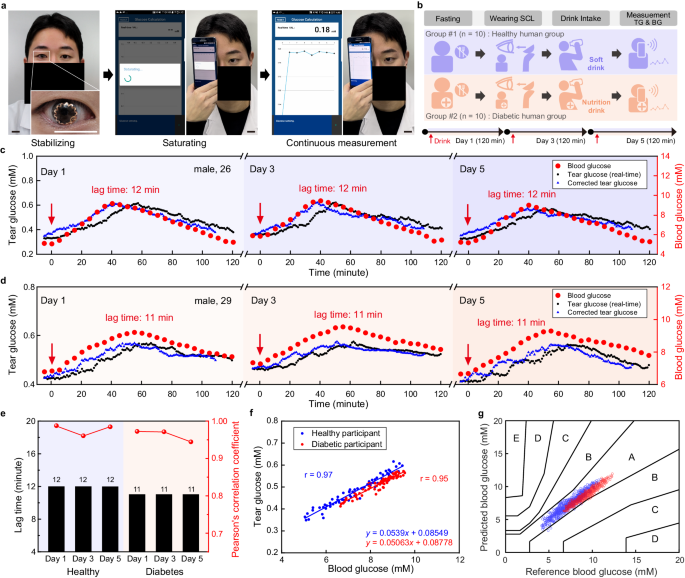
a Photographs of a human participant wearing smart contact lens (SCL) and TG measurement with SCL. Scale bars, 2 cm. Here, the participant’s face was blocked using a black bar, except for the eyes, to infringe the portrait right. b Human study protocol for healthy and diabetic participants. c Representative real-time data of monitoring TG and BG level in a healthy participant after intake of a soft drink on day 1, 3, and 5. d Representative real-time data of monitoring TG and BG levels in a diabetic participant after intake of a nutrition beverage on day 1, 3, and 5. e Comparison of lag time in each human participant on day 1, 3, and 5. f Pearson’s correlation analysis between TG and BG levels of each representative healthy and diabetic participant. g Comprehensive Parkes Error Grid analysis of ten healthy participants and ten diabetic participants.
Figure 5f shows the results of Pearson’s correlation analysis for a representative healthy and diabetic participant, which exhibited 0.97 and 0.95, respectively, as coefficient values. Such high levels indicate a positive correlation between TG and BG. The same analysis was performed for all remaining healthy and diabetic participants and the Pearson’s correlation coefficient over 0.9 was observed in each individual (Supplementary Figs. 31, 32). The comprehensive Parkes Error Grid analysis revealed that the predicted BG data points, derived from the TG data using each individual’s regression line equation, were all located within the A and B zones (Fig. 5g). This indicates that the prediction of BG level using our SCL was clinically accurate.


