Table of Contents
Diabetes It represents a complex spectrum of metabolic disorders and is primarily defined by hyperglycemia resulting from defects in insulin action, secretion, or both.
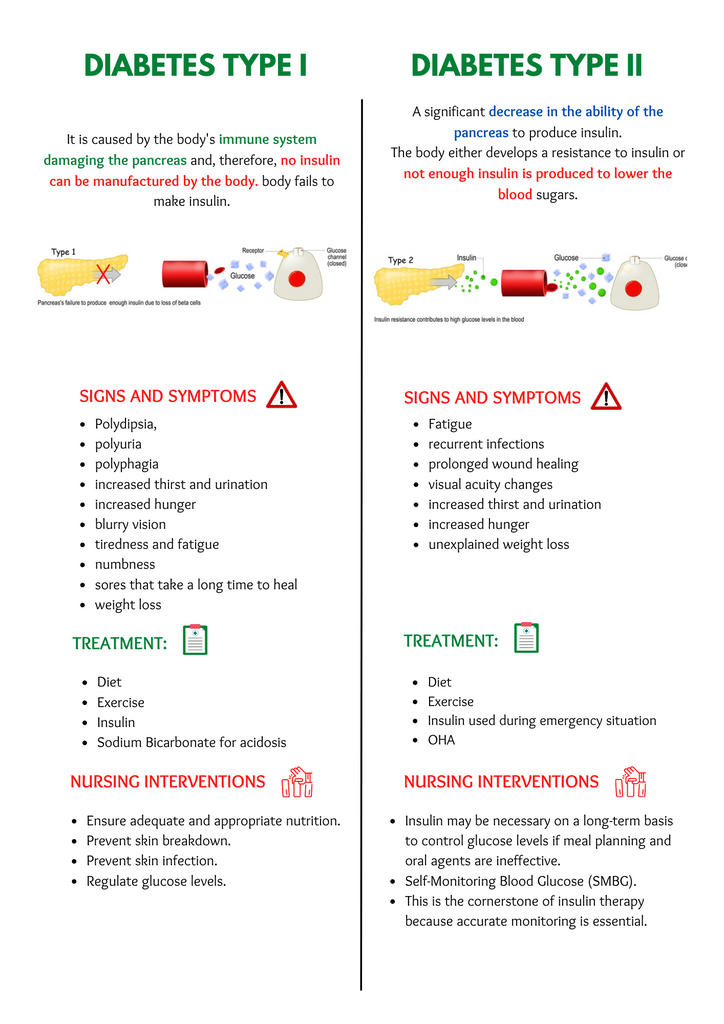
Type 1 diabetes (T1DM)) is primarily the result of autoimmune-mediated destruction. pancreatic islet beta cells, requires exogenous insulin for survival. This form of diabetes frequently appears in the pediatric population. However, it can develop at any age and is characterized by the rapid onset of the following symptoms: polyuria, polydipsia, polyphagiaand significant weight loss.
Type 2 diabetes mellitus (T2DM) mainly related to insulin resistance and relative insulin deficiency. The pathogenesis is multifaceted and involves a complex interaction between genetic predisposition and lifestyle factors. T2DM, which typically occurs in adults over the age of 35, is insidious and often goes undetected until complications occur. However, now, in parallel with the rising prevalence of obesity, more and more young people are being diagnosed with the disease. Clinical symptoms may be subtle or absent, but symptoms commonly include fatigue and recurrent infections.
gestational diabetes mellitus (GDM) This is a hyperglycemic condition detected during pregnancy and requires careful management to reduce maternal and fetal complications.
Additionally, certain forms of diabetes occur secondary to other medical conditions, such as: endocrine disease or pancreatic disease or caused by drugs.
prediabetes Refers to the intermediate metabolic stage in which an individual exhibits glucose intolerance or fasting blood sugar levels but does not meet the criteria for diabetes. At this stage, the risk of developing T2DM and cardiovascular disease increases.
Properly treating diabetes means knowing how the disease works in the body. While T1DM requires lifelong insulin therapy, management of T2DM ranges from dietary modifications to oral hypoglycemic agents and, in some cases, insulin supplementation. Nutritional status varies widely among diabetic patients and does not correspond to a single phenotype. Patients with T1DM or T2DM can range from underweight to obese.
in the area of endocrinology, diabetes management is individualized, taking into account the specific type, its etiology, the patient’s clinical profile, and the presence of comorbidities.Goals still need to be achieved euglycemia Prevent or manage complications and improve quality of life.
complications of diabetes
Understanding the complications of diabetes is essential for both clinical practice and patient education. Health issues related to diabetes span both acute and chronic conditions.
chronic complications It develops over time and can cause serious and irreparable damage if not properly managed.
- diabetic retinopathy: Diabetic retinopathy, a disease that affects the retina, can impair vision. Early detection through regular examinations is most important for treatment and prevention of vision loss.
- foot complications: Diabetes can lead to serious foot problems such as ulcers and infections, mainly due to nerve damage and poor circulation. Prompt attention to changes in sensation or appearance is important to prevent serious consequences such as amputation.
- cardiovascular complications: Sustained high blood sugar levels can damage blood vessels and increase your risk of heart attack and stroke.
- diabetic nephropathy: Diabetes can impair kidney function over time, making it difficult to manage water and waste products in the body, and is often exacerbated by high blood sugar and high blood pressure.
- neurological disorder: High blood sugar levels can cause neuropathy, affecting nerve signals and affecting vision, sensation, and movement.
- oral health problems: High blood sugar levels can increase sugar in saliva, which can lead to the growth of bacteria that cause tooth enamel erosion and periodontal disease. Damage to the blood vessels in the gums can increase susceptibility to infection.
- cancer risk: There is a notable correlation between diabetes and increased risk of certain diseases. type of cancer. Additionally, some cancer treatments can complicate diabetes management.
- sexual dysfunction: For women, diabetes reduces blood flow to the genitals, reducing sensation and increasing the risk of infections such as yeast infections and urinary tract infections. For men, damage to blood vessels and nerves can cause erectile dysfunction.
acute complicationsOn the other hand, it can occur suddenly and, if not treated in a timely manner, can lead to chronic symptoms. complications.
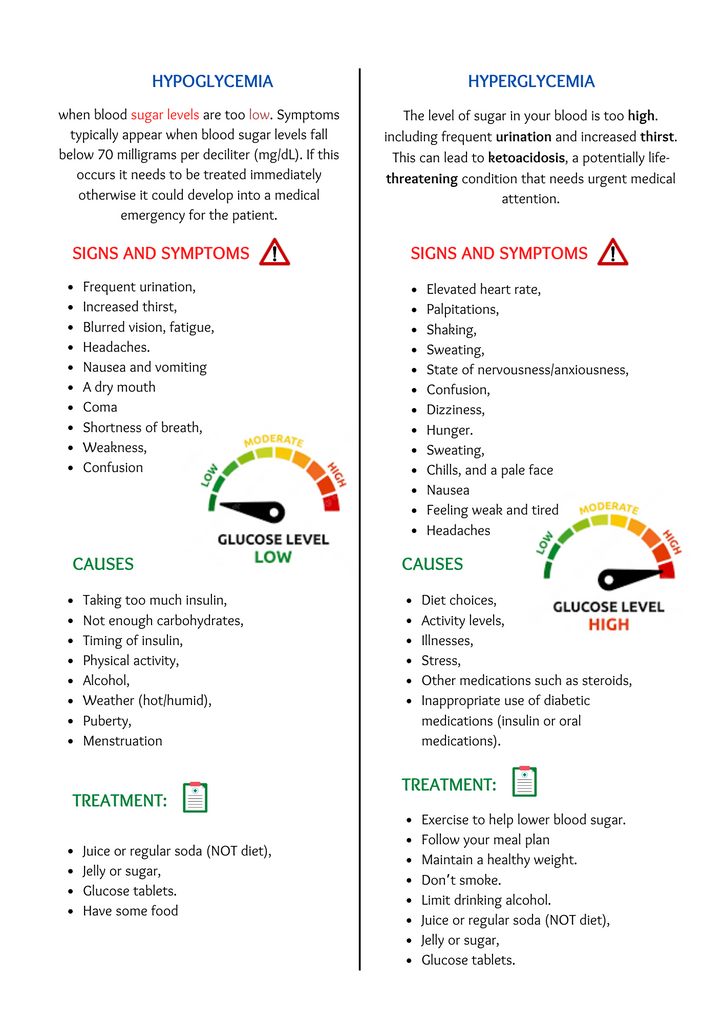
- hypoglycemia: Low blood sugar levels, or “hypoglycemia,” can occur quickly and require immediate treatment.
- hyperglycemia: High blood sugar, or “hyper,” can lead to serious conditions if untreated.
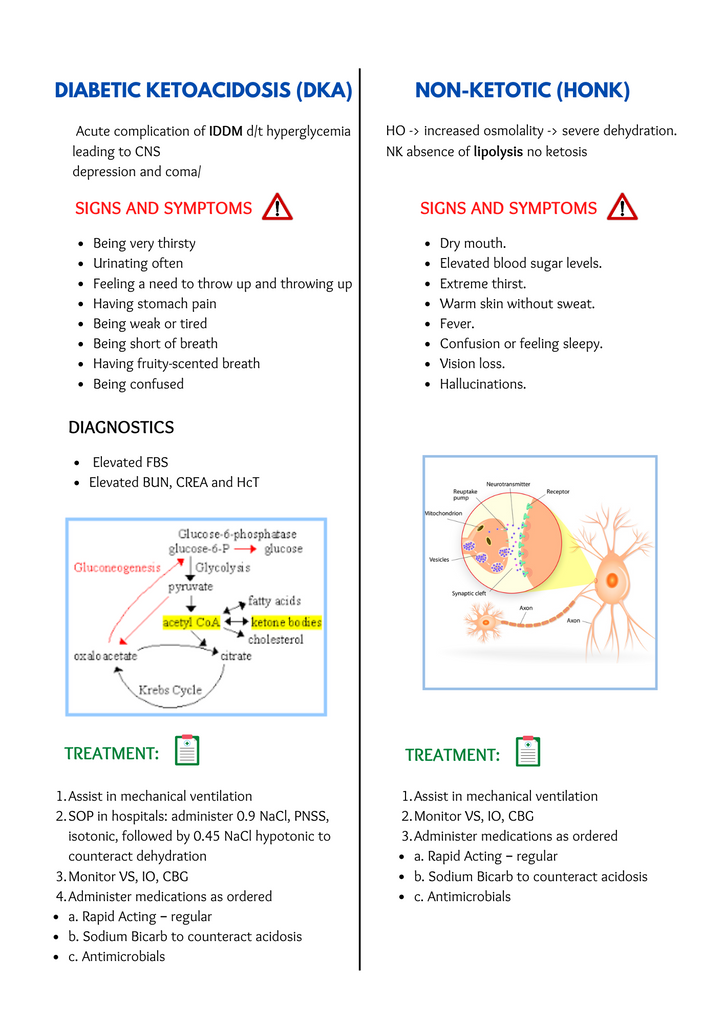
- Hyperosmolar hyperglycemic state (HHS): Formerly called HONK (hyperglycemic hyperosmolar nonketotic coma), this is a serious complication of diabetes, most common in type 2 diabetes, and caused by significant ketone levels in the body. Blood sugar levels rise rapidly even though the body is not present. blood or urine. Department of Health and Welfare It is a serious condition caused by severe dehydration and elevated blood sugar levels.
- Diabetic ketoacidosis (DKA): This is a serious, life-threatening condition primarily associated with type 1 diabetes, in which a lack of insulin causes a dangerous rise in blood sugar levels. This lack of insulin causes the body to break down fat for energy, producing acidic byproducts known as ketones. When ketone bodies build up, the blood becomes too acidic and the function of vital organs is inhibited. Early symptoms include intense thirst, frequent urination, vomiting, and nausea.
To prevent and manage these complications, people with diabetes must closely monitor their health, catch problems early, and make healthy lifestyle choices such as eating right and staying active. Must be. In some cases, you may need medicine to maintain your blood sugar levels and stay healthy.

The role of insulin in diabetes management
insulin, a hormone produced by the pancreas that helps the body store and use sugar and is important in regulating blood sugar levels. For people managing diabetes, it’s important to understand the different types of insulin and their timing. Rapid-acting insulin begins to lower blood sugar levels within 15 minutes and has a short duration of effect, making it suitable for controlling blood sugar during meals. Short-acting insulin works a little slower, starting within 30 minutes. Intermediate-acting insulins, including NPH, provide longer duration of glycemic control and are suitable as part of basal insulin therapy. Long-acting insulin mimics the body’s natural low-level insulin secretion, with no noticeable peaks and stable effects that last up to 24 hours. Understanding terms such as onset (when insulin starts to work), peak (when it is most effective), and duration (how long it remains effective) is essential for optimal diabetes management.

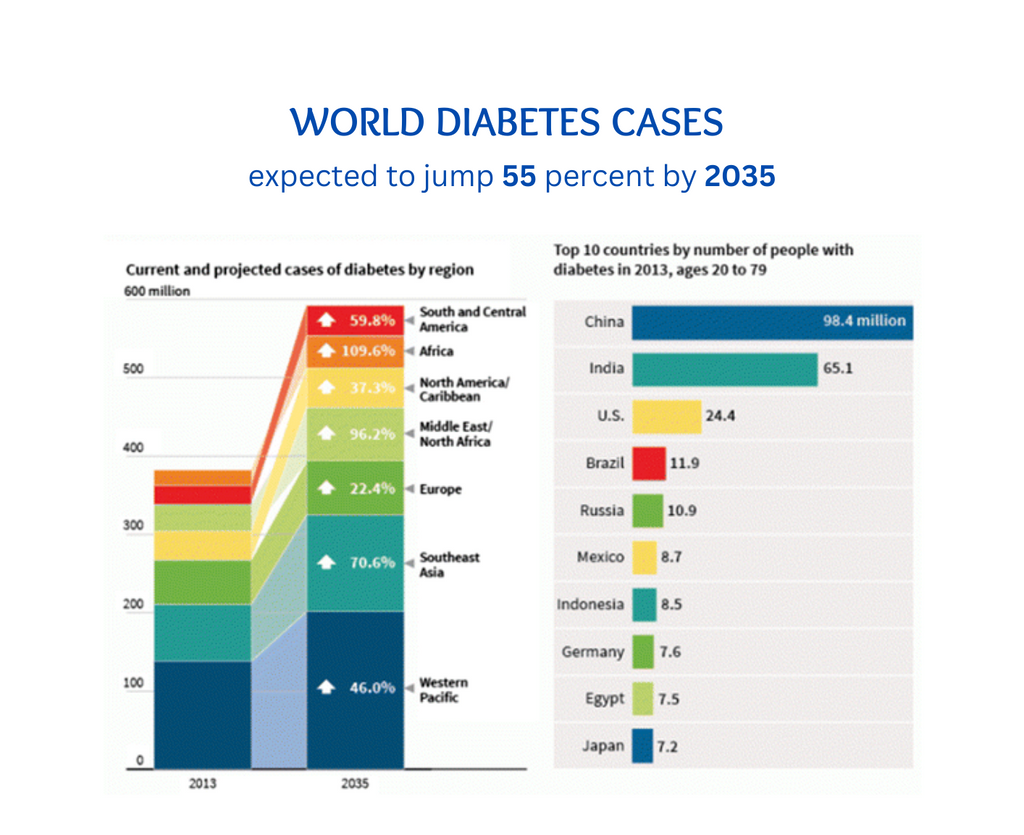
Number of diabetes patients in the world
By 2035, diabetes is expected to increase significantly. 55% increase in cases In the world. Currently, China and India have the highest number of diabetic patients. But it’s not just there. More cases are likely to occur in regions such as South America, Africa, and the Middle East. We need to be prepared by helping people live healthier lives and ensuring everyone has access to the care they need to prevent and treat diabetes.
A word from Viasox
Experience the ease of use of Viasox for diabetic foot care. Managing diabetes can be difficult, but support is always available. Relax, get support, and take care of yourself.via socks diabetic socks and compression socks Designed to provide foot comfort, increase blood circulation, and reduce foot complications. Trust Viasox to help you live a healthier, more comfortable life.


